FONTAN MECHANICS
Rafael Alonso-Gonzalez, MD, MSc
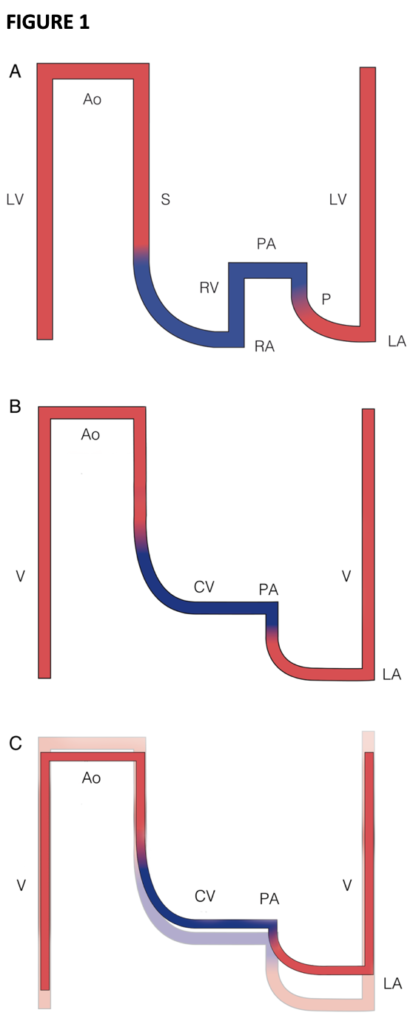
Figure 1- Scheme of the normal cardiovascular circulation (A), and the Fontan circulation at different stages (B and C). (A) Normal biventricular circulation: the pulmonary circulation (P) is connected in series to the systemic circulation (S). The compliance of the right ventricle ensures that the right atrial pressure remains lower than the left atrial pressure and delivers the driving force to the blood to overcome pulmonary impedance. (B) Fontan circuit: the caval veins are directly connected to the PA; systemic venous pressures are markedly elevated. (C) Fontan circuit late (superimposed on early Fontan circuit): with time, a negative spiral ensues: pulmonary resistance increases resulting in further increase in CV congestion but even more in reduced flow, which increases ventricular filling pressure. Ao, aorta; CV, caval veins; LA, left atrium; LV, left ventricle; PA, pulmonary artery; RV, right ventricle; V, single ventricle. Line thickness reflects output, and colour reflects oxygen saturation. Reproduced with permission from Gewillig M, Brown SC.2
A normal mammal cardiovascular system consists of a double circuit, pulmonary and systemic, connected in series and powered by a double pump, the right and left ventricles (Figure 1A).
However, multiple congenital heart malformations have only a single pumping chamber supporting both circulations. In this setting, the circulations are connected in parallel causing significant desaturation, at rest and with exercise, and chronic volume overload of the single ventricle. Chronic volume overload will lead to deterioration of the ventricular function and ultimately to heart failure.
In 1971, Francis Fontan described an intervention to separate the systemic and pulmonary circulations in patients with a single ventricle. This intervention is known as ‘Fontan procedure’ and although there have been multiple modifications of the original operation, the mechanics of the ‘Fontan circulation’ remain the same. In a ‘Fontan circulation’ the systemic venous return is connected to the pulmonary arteries without the interposition of an adequate ventricle, and the postcapillary energy is used to drive blood through the lungs. The pulmonary impedance hampers venous return through the pulmonary vascular bed leading to congestion upstream and restricted flow downstream. The latter will cause reduction in preload reserve to the ventricle and subsequently, reduction in cardiac output.
By creating a ‘Fontan circulation’ a new portal system is made (Figure 1B). A portal system occurs when one capillary bed pools blood into another capillary bed through veins without passing through the heart.
The ‘Fontan circulation’ has two main components:
(a) the single ventricle that pumps blood to the systemic circulation
(b) the systemic venous return that will reach the pulmonary arterial system without a pumping chamber.
The driving force that maintains adequate blood flow in the circuit is the pressure difference between the central venous pressure and common atrial pressure, also known as transpulmonary gradient. Maintaining an optimal transpulmonary gradient requires a good function of the single ventricle, a low afterload and an appropriate preload.
The cardiac output in a ‘Fontan circulation’ relies on non-pulsatile, passive flow of the systemic venous return to the pulmonary arteries and is decreased to approximately 70%. The absence of a subpulmonary ventricle makes the circulation to rely on low pulmonary pressure and low pulmonary vascular resistance. Whereas ventricular contractility is one of the main drivers of cardiac output in patients with biventricular circulation, pulmonary vascular resistance is the main determinant of cardiac output in patients with ‘Fontan circulation’. Ventricular function is important only when it is severely depressed. Systemic venous pressure also affects cardiac output although to a lesser degree. Patients with ‘Fontan circulation’ need some degree of venous hypertension to maintain adequate transpulmonary blood flow, hence systemic venous pressure is slightly higher in these patients. However, systemic venous pressures above 20 mmHg are likely to lead to systemic venous congestion and subsequently reduce cardiac output. Any significant gradient in the Fontan circuit should be addressed to prevent reduction of the single ventricle preload. Over time, there will be a steady increase in central venous pressure, pulmonary vascular resistance and ventricular filling pressure, resulting in a progressive reduction in cardiac output (Figure 1C).
Close surveillance of patients with ‘Fontan circulation’ is paramount to maintain optimal functioning of the Fontan circuit. It is important to maintain good body weight, avoid smoking and to engage in physical activity. Recent studies suggest that regular exercise contributes to improve the function of the pulmonary circulation and may also improve the diastolic function of the single ventricle. The role of pulmonary vasodilators in the setting of ‘Fontan circulation is currently under investigation.
View References- Gewillig M. The Fontan circulation. Heart 2005;91:839–846.
- Gewillig M, Brown SC. The Fontan circulation after 45 years: update in physiology. Heart. 2016;102:1081-6.
- Ohuchi H. Adult patients with Fontan circulation: What we know and how to manage adults with Fontan circulation? J Cardiol. 2016;68:181-9.
- Gewillig M, Brown SC, van de Bruaene A, Rychik J. Providing a framework of principles for conceptualising the Fontan circulation. Acta Paediatr. 2020;109:651-658.
- Gewillig M, Brown SC, Eyskens B, Heying R, Ganame J, Budts W, La Gerche A, Gorenflo M. The Fontan circulation: who controls cardiac output? Interact Cardiovasc Thorac Surg. 2010;10:428-33.
- Cordina R, d'Udekem Y. Long-lasting benefits of exercise for those living with a Fontan circulation. Curr Opin Cardiol. 2019;34:79-86.
- Cordina R, Celermajer DS, d'Udekem Y. Lower limb exercise generates pulsatile flow into the pulmonary vascular bed in the setting of the Fontan circulation. Cardiol Young. 2018;28:732-733.

